Below is a guest post by Lynsey Keator, MA, CCC-SLP. Lynsey is a speech-language pathologist who currently works with Dr. Argye Hillis at Johns Hopkins. She will be joining the USC Aphasia Lab in the Fall to begin her doctoral work. Her post summarizes a recently published article, “Predicting Recovery in Acute Poststroke Aphasia.” This article appears in the journal, Annals of Neurology. Link to the full article here: https://onlinelibrary.wiley.com/doi/full/10.1002/ana.25184
Study Background and Purpose
Immediately after a stroke, many patients suffer from severe language-related impairments. Word finding is one of the most common difficulties. Problems with word finding significantly affect communication in daily life. Despite initial difficulties, many individuals regain naming abilities in the months after a stroke. However, it is difficult to predict which of patients will show good recovery, little recovery, or even decline.
The goal of this study was to identify which patients may show better recovery on naming tasks. Previous research has identified two variables associated with good recovery of naming:
- Damage to specific areas of the brain associated with language
- Use of antidepressants
Specifically, this study focused on the impact of
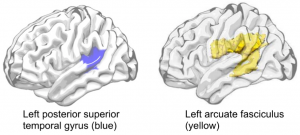
- Damage in the left posterior superior temporal gyrus (pSTG) and superior longitudinal fasciculus/arcuate fasciculus (SLF/AF) (see images below)
- Use of selective serotonin reuptake inhibitors (SSRIs) on aphasia recovery.
Hypotheses
We hypothesized that:
- Patients without damage in these two areas demonstrate better recovery than those with damage to the pSTG and SLF/AF.
- Even if individuals have damage to these areas, they may show positive outcomes after taking an SSRI daily for three months post stroke.
We were specifically interested in observing changes in naming ability in early recovery (days post-stroke) and in the chronic stage (at least 6 months post-stroke).
Results
The results of this study showed:
- Damage to the left pSTG and SLF/AF predict naming performance months after a stroke. Findings suggest damage to these areas lead to worse later recovery. While these areas are not exclusively responsible for naming, the results confirm they serve a substantial role in this domain of language.
- Patients with damage to these same areas show improved recovery of naming with the use of SSRIs. This suggests outcomes for may be improved by the use of SSRIs. This finding is consistent with previous studies that have demonstrated positive effects of SSRIs on motor recovery and cognitive function, independent of depression.
Why is this research important?
This and continued research is critical because it helps to identify important factors related to language recovery after a stroke. With a greater consideration of lesion location, especially areas related to language recovery, clinicians can provide an accurate prognosis, personalized treatment approach, and plan of care.
Additionally, the positive effects of SSRIs on cognitive function, motor recovery, and naming independent of depression may be important for clinicians and families to consider in the acute and sub-acute periods of recovery.